Delve into the intricacies of ATI real life kidney disease, a condition that affects the kidneys and can lead to serious health complications. This guide will provide an overview of the causes, symptoms, diagnosis, and treatment options for this condition, empowering you with the knowledge to manage your health effectively.
ATI, or Acute Tubular Interstitial Nephritis, is a type of kidney disease that affects the tubules, which are tiny structures in the kidneys responsible for filtering waste products from the blood. When these tubules become inflamed or damaged, they can no longer function properly, leading to a buildup of toxins in the body and a decline in kidney function.
Etiology of Acute Tubular Interstitial Nephritis (ATI)
Acute tubular interstitial nephritis (ATI) is an inflammation of the tubules and interstitium of the kidney. It can be caused by a variety of factors, including toxins, medications, infections, and autoimmune disorders.
Toxinsthat can cause ATI include heavy metals (such as lead and mercury), organic solvents (such as trichloroethylene and carbon tetrachloride), and drugs (such as cocaine and heroin).
Medicationsthat can cause ATI include antibiotics (such as aminoglycosides and vancomycin), nonsteroidal anti-inflammatory drugs (such as ibuprofen and naproxen), and diuretics (such as furosemide and hydrochlorothiazide).
Infectionsthat can cause ATI include bacteria (such as Streptococcusand Staphylococcus), viruses (such as cytomegalovirus and Epstein-Barr virus), and fungi (such as Candidaand Aspergillus).
Autoimmune disordersthat can cause ATI include lupus, Sjogren’s syndrome, and rheumatoid arthritis.
Ischemia, or a lack of blood flow to the kidneys, can also lead to ATI. This can occur in conditions such as shock, sepsis, and heart failure.
Sepsis, a severe infection that can lead to organ failure, is a common cause of ATI. The inflammatory response to sepsis can damage the kidneys, leading to ATI.
ATI Real Life Kidney Disease, a condition affecting many, can be debilitating. To understand the complexities of this disease, we can draw parallels to the theological debates surrounding Is Ben Stuart a Calvinist . Just as the tenets of Calvinism shape religious beliefs, so too do the intricacies of kidney disease influence the lives of those affected, highlighting the profound impact of both physical and spiritual ailments on our well-being.
| Etiology | Incidence | Risk Factors |
|---|---|---|
| Toxins | 10-20% | Exposure to heavy metals, organic solvents, or drugs |
| Medications | 10-15% | Use of antibiotics, NSAIDs, or diuretics |
| Infections | 10-15% | Bacterial, viral, or fungal infections |
| Autoimmune disorders | 5-10% | Lupus, Sjogren’s syndrome, or rheumatoid arthritis |
| Ischemia | 5-10% | Shock, sepsis, or heart failure |
| Sepsis | 5-10% | Severe infection |
Pathophysiology of ATI: Ati Real Life Kidney Disease
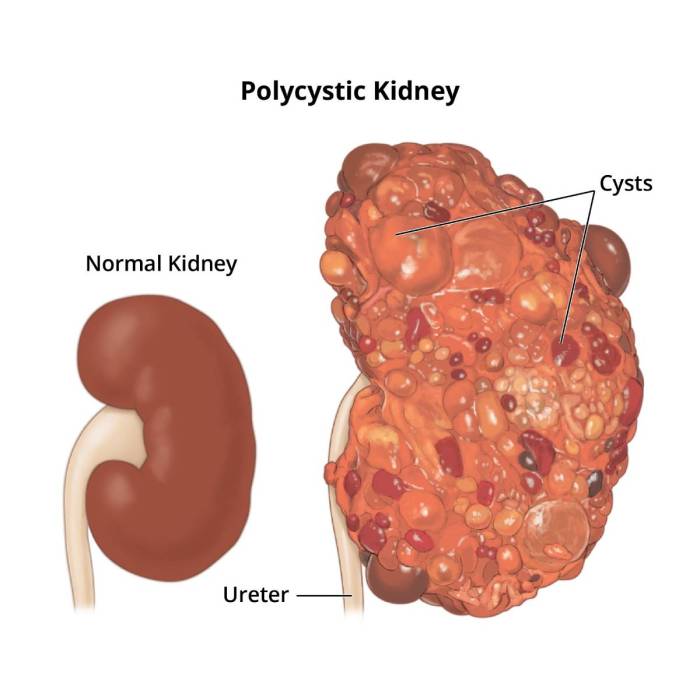
Acute tubular interstitial nephritis (ATI) is a condition characterized by inflammation and injury to the tubules and interstitium of the kidneys. The pathophysiology of ATI involves a complex interplay of cellular and molecular mechanisms, including inflammation, oxidative stress, and apoptosis.
Inflammation, Ati real life kidney disease
Inflammation plays a central role in the development of ATI. In response to various insults, such as toxins, drugs, or infections, inflammatory cells, including neutrophils, macrophages, and lymphocytes, infiltrate the kidney tissue. These cells release pro-inflammatory cytokines and chemokines, which further amplify the inflammatory response and promote tissue damage.
Oxidative Stress
Oxidative stress occurs when there is an imbalance between the production of reactive oxygen species (ROS) and the body’s antioxidant defenses. In ATI, excessive ROS production can lead to lipid peroxidation, protein oxidation, and DNA damage, contributing to tubular cell injury and apoptosis.
Apoptosis
Apoptosis, or programmed cell death, is another important mechanism involved in ATI. Tubular cells can undergo apoptosis in response to various stimuli, including inflammation, oxidative stress, and direct cytotoxic injury. Apoptosis leads to the orderly dismantling of the cell, preventing the release of harmful intracellular contents and inflammation.
Stages of ATI
ATI typically progresses through several stages:
- Initiation:Triggered by an inciting event, such as exposure to a toxin or infection, leading to inflammation and oxidative stress.
- Progression:Inflammatory response intensifies, tubular cells undergo apoptosis, and interstitial fibrosis develops.
- Recovery:If the inciting event is removed, inflammation resolves, tubular cells regenerate, and fibrosis may regress.
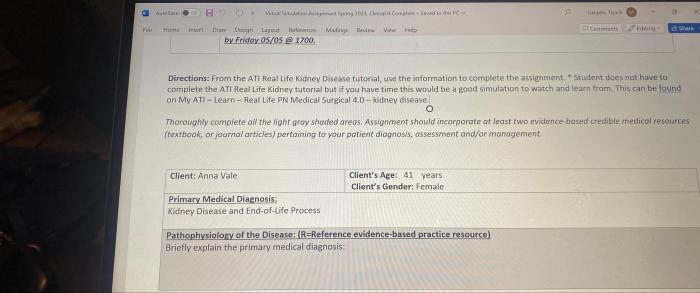
Clinical Manifestations of ATI
Acute tubular interstitial nephritis (ATI) is a condition characterized by inflammation of the tubules and interstitium of the kidneys. The clinical manifestations of ATI can vary depending on the severity of the injury and the underlying cause.
Clinical Signs and Symptoms
Common clinical signs and symptoms of ATI include:
- Oliguria (decreased urine output)
- Polyuria (increased urine output)
- Electrolyte disturbances (e.g., hyperkalemia, hyponatremia)
- Edema (swelling)
- Fatigue
- Nausea and vomiting
- Flank pain
- Fever
Laboratory Tests
Laboratory tests can help diagnose ATI and assess the severity of the injury. Common laboratory tests used include:
- Serum creatinine: Elevated serum creatinine levels indicate impaired kidney function.
- Urine analysis: Urine analysis may reveal proteinuria (presence of protein in the urine), hematuria (presence of blood in the urine), and casts (cylindrical structures formed in the kidney tubules).
- Electrolyte panel: Electrolyte disturbances, such as hyperkalemia and hyponatremia, are common in ATI.
Differential Diagnosis
ATI must be differentiated from other causes of acute kidney injury, such as:
- Prerenal azotemia (decreased blood flow to the kidneys)
- Postrenal azotemia (obstruction of urine flow)
- Glomerulonephritis (inflammation of the glomeruli)
- Pyelonephritis (infection of the kidneys)
The diagnosis of ATI is based on a combination of clinical findings, laboratory tests, and imaging studies.
Management of ATI
The management of ATI involves a multifaceted approach, encompassing supportive care, targeted treatment of the underlying cause, and specific therapies to mitigate the inflammatory response and promote renal recovery.
Supportive Care
Supportive care measures aim to maintain fluid and electrolyte balance, prevent complications, and optimize overall patient well-being. This includes:
- Intravenous fluids to maintain adequate hydration and correct electrolyte imbalances.
- Electrolyte monitoring and replacement to prevent electrolyte disturbances.
- Nutritional support to ensure adequate calorie and protein intake.
- Monitoring for and management of complications such as sepsis, electrolyte imbalances, and acute kidney injury.
Treatment of the Underlying Cause
Identifying and treating the underlying cause of ATI is crucial to prevent further renal damage. This may involve:
- Antibiotics for bacterial infections.
- Antifungals for fungal infections.
- Immunosuppressive agents for autoimmune disorders or drug-induced ATI.
- Removal of nephrotoxic agents or medications.
Specific Therapies
In addition to supportive care and treatment of the underlying cause, specific therapies may be employed to reduce inflammation and promote renal recovery. These include:
- Diuretics to enhance urine output and reduce fluid retention.
- Loop diuretics such as furosemide are commonly used to promote diuresis.
- Immunosuppressive agents such as corticosteroids may be used to suppress inflammation in severe cases.
Prognosis of ATI
The prognosis of ATI varies depending on the severity of the injury, the underlying cause, and the patient’s overall health. In general, patients with mild ATI have a good prognosis and recover fully within a few weeks. However, patients with severe ATI may experience long-term complications, including chronic kidney disease (CKD) and end-stage renal disease (ESRD).
Factors Influencing Prognosis
The following factors influence the prognosis of ATI:*
-*Severity of the injury
The more severe the injury, the worse the prognosis. Patients with severe ATI are more likely to develop CKD and ESRD.
-
-*Underlying cause
The underlying cause of ATI can also affect the prognosis. Patients with ATI caused by a treatable condition, such as an infection, have a better prognosis than patients with ATI caused by a non-treatable condition, such as a genetic disorder.
-*Patient’s overall health
The patient’s overall health can also affect the prognosis of ATI. Patients with other medical conditions, such as diabetes or high blood pressure, are more likely to develop complications from ATI.
Long-Term Outcomes
The long-term outcomes of ATI can vary depending on the severity of the injury. Patients with mild ATI typically recover fully and have no long-term complications. However, patients with severe ATI may experience long-term complications, including:*
-*Chronic kidney disease (CKD)
CKD is a condition in which the kidneys are damaged and cannot function properly. CKD can lead to a number of health problems, including high blood pressure, heart disease, and stroke.
-*End-stage renal disease (ESRD)
ESRD is the most severe form of CKD. ESRD occurs when the kidneys are no longer able to function on their own. Patients with ESRD require dialysis or a kidney transplant to survive.
Prognostic Factors and Outcomes of ATI
The following table summarizes the prognostic factors and outcomes of ATI:| Prognostic Factor | Outcome ||—|—|| Severity of the injury | Worse prognosis with severe injury || Underlying cause | Better prognosis with treatable causes || Patient’s overall health | Worse prognosis with other medical conditions || Long-term outcomes | Mild ATI: typically no long-term complications || | Severe ATI: may develop CKD or ESRD |
Popular Questions
What are the common causes of ATI?
ATI can be caused by various factors, including exposure to toxins, certain medications, infections, and autoimmune disorders.
What are the symptoms of ATI?
Symptoms of ATI may include decreased urine output, increased thirst, fatigue, nausea, and swelling in the legs or ankles.
How is ATI diagnosed?
ATI is diagnosed through a combination of physical examination, blood tests, and urine analysis.
What are the treatment options for ATI?
Treatment for ATI typically involves supportive care, such as managing fluid and electrolyte balance, and addressing the underlying cause of the condition.
What is the prognosis for ATI?
The prognosis for ATI depends on the severity of the condition and the underlying cause. Early diagnosis and treatment can improve outcomes and prevent long-term kidney damage.